Writing for The Guardian on 9 November 2015, Dr Ranjana Srivastava, an Australian oncologist and author ('After Cancer: A Guide to Living Well') gives an insight into her experience of the place of euthanasia in patients' concerns and needs:
In 15 years of practising medicine, I have had one conversation about euthanasia and a handful about medical marijuana. Alternative therapy comes up most days but the vast majority of my conversations as an oncologist are about prolonging life. They are about doing the utmost to extract the last drops from a finite life, if not for their own sake then for the sake of a child's graduation, a grandchild's birth, a friend's wedding.
The miracle my patients yearn for is not deliverance from their terrible disease but a little more time to cherish life, with all its shortcomings. They say that the drudgery of life beats the anonymity of death.
Her piece is an honest consideration of how her profession engages with the end of life, and she is frank about the sometimes haphazard nature of care for people with incurable conditions:
When discussing euthanasia, heavy emphasis is put on the word "voluntary". Yet we know that a host of everyday decisions taken by patients raise questions about their true voluntariness. Sure, patients will sign consent forms and nod at instructions but it's easily and painfully evident how little they really understand about the consequences of their decisions. This is not to diminish their acumen but simply to observe that health literacy is woeful and thus its corollary is deep trust in a doctor's word. Shared decision-making is laudable but one of the most frequent phrases in medicine remains, "You're the doctor, you know best."
Scant explanation and poor understanding of their options leads patients to give consent for unjustified procedures but also to forego necessary interventions. A geriatrician recently saved the life of an elderly patient who had been denied powerful antibiotics for her pneumonia because others did not deem her wheelchair-bound life worth living. The woman had simply accepted that she had an incurable condition and was ready to die.
An acutely confused octogenarian was shunted to a secluded nursing home by his self-appointed guardian who coveted his estate. A vigilant nephew realised that a mockery had been made of the informed consent process in a hospital that had been more interested in processing him than caring for him.
Her experience of caring for people facing death was that many of those for whom others wish to speak in this debate wish simply to hope and strive to stay alive:
The majority of my patients are dying, therefore conversations about how they will die are routine. Since so many patients are poor, malnourished, illiterate and socially disadvantaged in every imaginable way, their end of life experience can be particularly fraught. But I am continually surprised by their tenacity and spirit and the will to live. They don't deny their impending fate but derive comfort from simple acts of love and care. Even in their final days, they thrive on friendship and community. Despite wanting a miracle cure and hearing there isn't one, my patients don't want to hasten death. I daresay many would be perplexed by the notion of euthanasia... There is a particularly good reason to tune in to the quieter voices and heed the needs of the traditionally marginalised.
Again, she is frank about what modern medicine can offer at the end of life, but argues that what many see as a failing of medicine in alleviating suffering is in fact a failing of society to support and comfort each other not as patients, but simply as human beings:
Palliative care does not and cannot relieve everyone's symptoms all the time. It's also better at relieving physical symptoms than addressing existential anguish. And yet, it is this anguish that is universal, which pills and potions can't banish. Why now, why me? What has my child done to deserve this fate? How can I survive war but get cancer? And just as existential anguish stems from being human, communion with fellow humans turns out to be the best antidote.
The terminally ill patients who suffer doubly are those who are ostracised by their relatives, estranged from their children, divorced by their spouse and left to shoulder their burden alone. There is no easy solution to this intractable problem, which is really a failure of modern society and its fraying relationships rather than a limitation of medicine. Downplaying the value of palliative care will confuse patients and do them a disservice.
Dr Srivastava's comment piece is well worth reading in full.
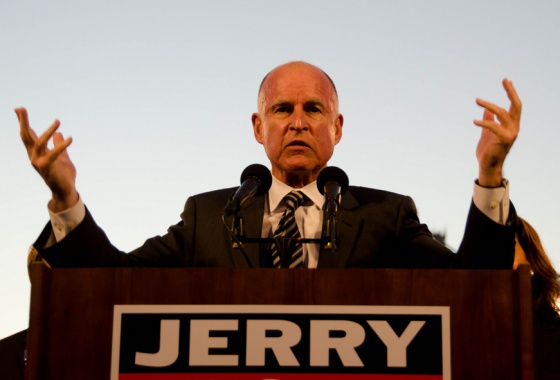
(Image: Twitter)